Is it your adductors? It's probably your adductors.
Sneaky inner thigh muscles are all up in your pelvic floor.
I have this visceral memory of how my body experienced anxiety as a child: as a young kid (six? Who’s to say!?) I would reflexively lock my knees and squeeze the ever-loving shit out of my quads and inner thighs. Anything could trigger this response — the car stopping short, being caught while telling a lie, test anxiety — anything.
Everyone has their own unique physical responses to stress. But squeezing the inner thighs and/or pelvic floor are pretty common ones for all the reasons — if we’re getting Freudian about it, closing down the pelvic space is a key way to both protect the body and exert control.
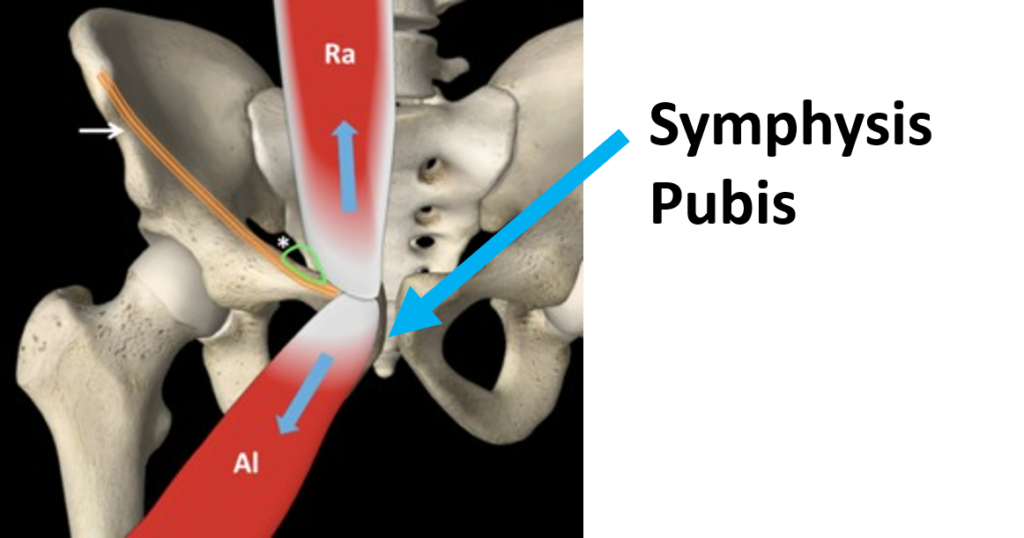
Just like the glutes and the psoas, the adductors are another common culprit to consider when we consider pelvic floor dysfunction: particularly pelvic pain, incontinence, urgency, and pubic symphysis pain. So let’s get into it.
Here’s the tl;dr:
The adductors, abdominal muscles, and pelvic floor share fascial and nerve ending connections, meaning that they often co-contract together. That means if the adductors are engaging, the pelvic floor is, too.
The adductors attach to the pubic bone, meaning that tension can contribute to pelvic girdle pain, especially in pregnancy (but also always).
While it’s tempting to think that strengthening the crap out of the adductors would create a pristine pelvic floor, we all know it’s not that simple. We’re going for strong and resilient, folks!
Relevant reading:
Move your ass. On glutes, my favorite!
The not so mythical psoas and why it’s probably still creating drama for your bod. I feel like that title is all you need.
WTF is up with lightning crotch? If you’ve ever experienced that bolt of pain in the center of your pelvis, this is for you.
The deep dive:
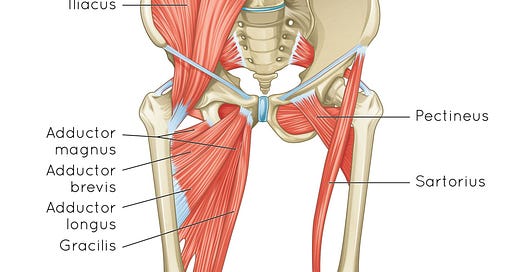
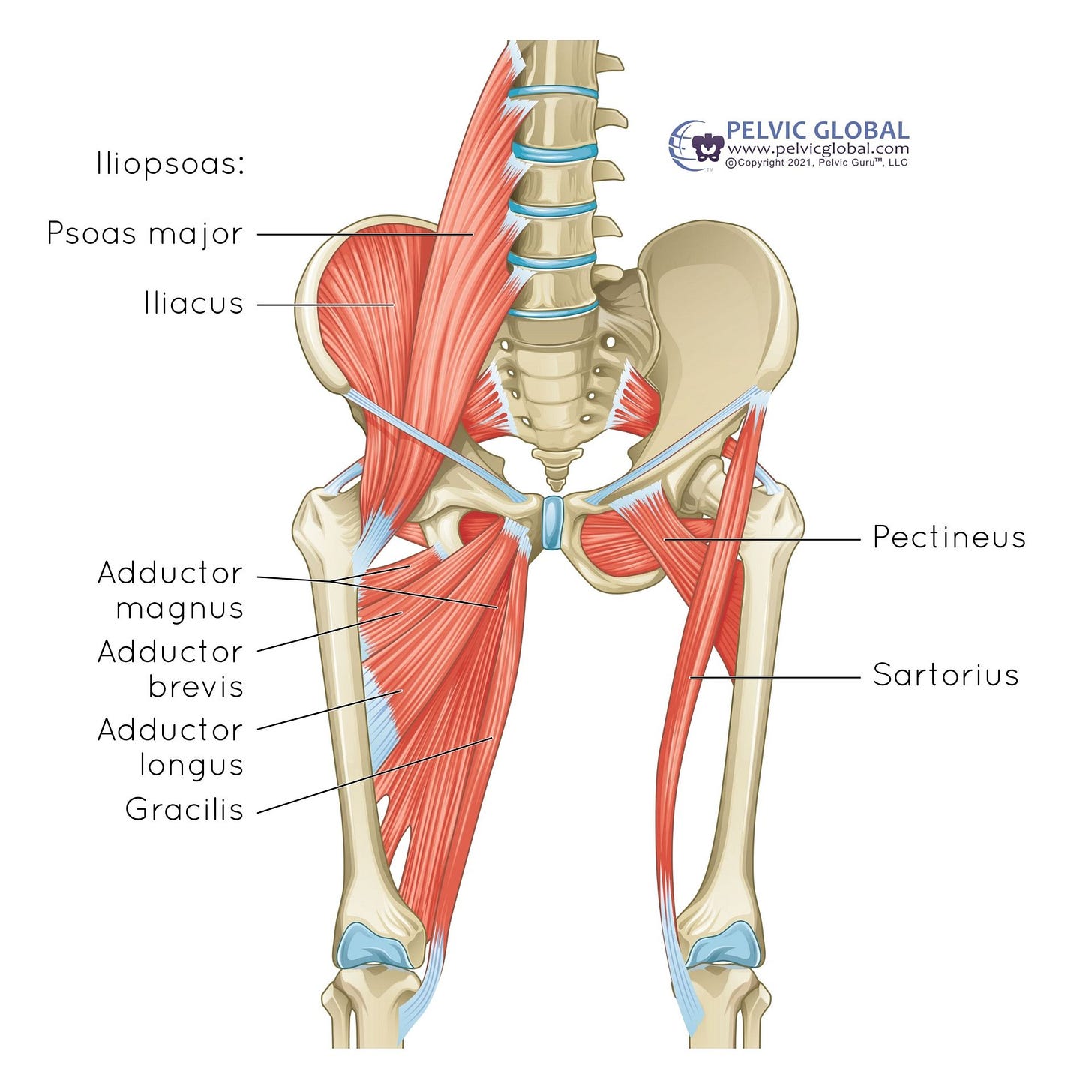
As always, let’s begin with anatomy:
Okay, cool. So we can see how we’re looking at a functional group of muscles (both quite long and incredibly short) that all attach to the pubic symphysis.
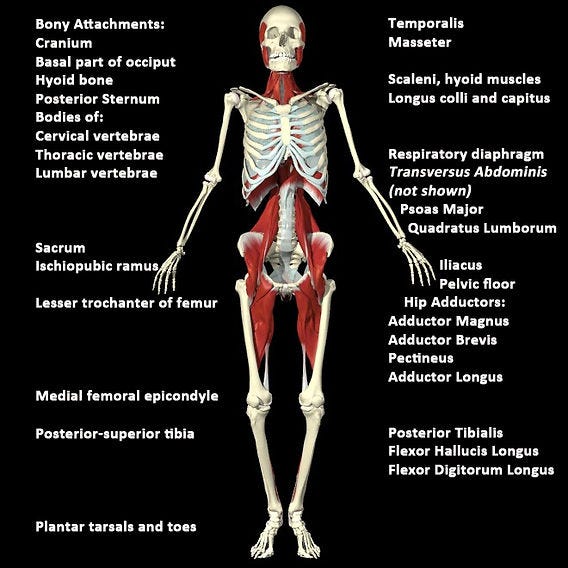
From a fascia perspective, we’re looking at “the deep front line”:
Side bar: Kind of nuts, when we consider the clinical connection between temporomandibular junction dysfunction (TMJ) and pelvic pain, to see this line, huh?
Okay, moving on:
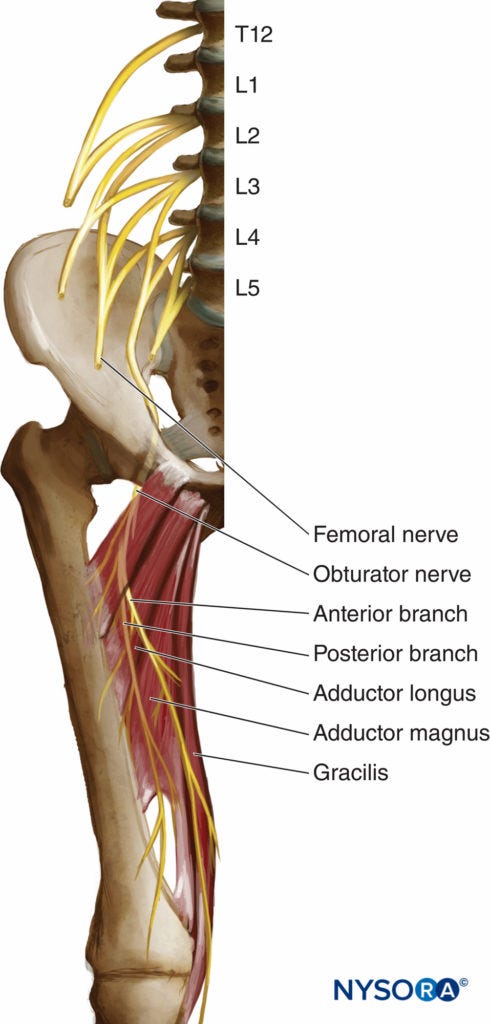
Don’t stress out about the specific nerve anatomy, but instead marvel at the fact that these nerves are making an epic journey from the spine, through the pelvis, and into… the adductors. Which is why one of the first assessments many clinicians (myself included) do on an internal pelvic exam is to test whether the skin of inner thighs stimulates any pain in the pelvis.
So wtf does this mean from a clinical perspective? Here are the scenarios where I think about adductors the most:
Pelvic floor tension and pain (especially vaginismus/vulvodynia, but any kind of pelvic floor pain): Adductors are often hella tight with any kind of pelvic floor pain where the body needs to protect itself from pain. A guarding response via the adductors can be pretty strong when someone with a history of pelvic pain and/or trauma experiences any perceived threat. This can create a vicious cycle of sorts, where a guarding response feeds forward to chronic tension in the adductors and thus even more tension in the pelvic floor.
Often, when folks with pelvic pain aren’t up for internal work (valid!) — and even when they are! — we can make crazy progress by working on releasing and sustainably lengthening the adductors and abdominals because of the aforementioned fascial connection. Break the vicious cycle of muscle guarding, make progress no dilator ever could!
Pubic symphysis pain (SPD): Fondly referred to as “lightning crotch”, this is super duper common in pregnancy. I like to refer to pregnancy as a losing war in physics, because, well, it is. There’s some psychotically fast growth happening in the abdomen that creates a significant pull on the lumbar spine and pelvic girdle, and tension in the adductors is pretty par for the course, putting a direct pull on — you guessed it — the pubic symphysis.
Treating SPD usually involves more eccentric strengthening of the adductors instead of stretching (which can put more pull on the pubic joint).
Incontinence and urinary urgency: Raise your hand if you’ve ever instinctively crossed your legs or squeezed your inner thighs to try to hold in pee. If so, you already understand the co-contracting relationship of the adductors to the pelvic floor. Go you! It’s true that adductors can help hold in pee in a pinch. But this relationship gets to be more trouble than it’s worth when we over-utilize the adductors instead of actually coordinating and strengthening the pelvic floor. Worse, we get into the same vicious cycle as we did when there’s pelvic pain: squeezing the shit out of your inner thighs just creates a more rigid, tense, and ultimately not very strong pelvic floor or adductor complex.
I have also seen absolute magic happen when we create length in the medial adductors — those little fuckers like pectineus and adductor brevis can get really grippy and create havoc in the pelvic floor. If your pelvic floor is relatively strong and you’re still experiencing random stress urinary incontinence, this is worth checking out!
Here’s the take-home:
There’s actually no one way to release the adductors. Like everything else to do with bodies, it’s all about choosing the right intervention for the right person at the right time. Here are some strategies I use in my practice:
Manual release: This is a preferred strategy of mine in the case of vaginismus and SPD. If you don’t have access to a provider, using a foam roller or release ball can be helpful, too!
Passive release: My favorite way to stretch, this involves a low intensity, often supported stretch for a longer period of time (think 2-5 minutes). This strategy creates an effect called “creep” where the muscle adapts from a neuromuscular perspective over time and therefore actually lengthens and changes. Love that for us!
Dynamic stretching: This can come in super handy when we’re addressing difficult to reach muscles, like the shorter adductor muscles.
Eccentric strengthening: Particularly helpful when we’re considering instability in the pelvis (like in the case of SPD and pregnancy) but also all the time when we’re retraining the adductors to stay in a lengthened, strong state. Similarly, strengthening the adductors can be helpful when managing incontinence — but instead of clamping down, squeezing the crap out of them, and hoping for the best, we’re creating a strong, resilient, and reflexive adductor system to compliment the equally resilient and reflexive pelvic floor.
If you’re not sure what your body needs, that’s where getting an assessment can be helpful. I will also be posting a full spectrum adductor practice on Thursday so that you can get a sense of what resonates best in your body! (This is for paid subscribers only — subscribe or upgrade your subscription now so it comes straight to you!)
I love hearing from you. Respond to this email or comment below and tell me what’s on your mind! As always, I am rooting for you.